What’s Public Health Got to Do With…HIV and Aging?

by Dorcas Baker, RN, BSN, ACRN, MA
Regional Coordinator, JHU AIDS Education and Training Center
Center for Infectious Disease and Nursing Innovation
Johns Hopkins University School of Nursing
With high-quality care and successes of HIV treatment over the past three decades, people diagnosed with HIV now have a nearly normal life expectancy. Today, more than half of people living with HIV in the United States are aged 50 or older, and a growing number of people are living and aging with HIV into their 70’s and beyond. According to the Centers for Disease Control and Prevention (2020), people living with HIV (PLWH) in the U.S. accounted for 17% of new diagnoses in 2016. Although this is a public health success, living longer with HIV also presents additional, and sometimes highly complex, challenges.
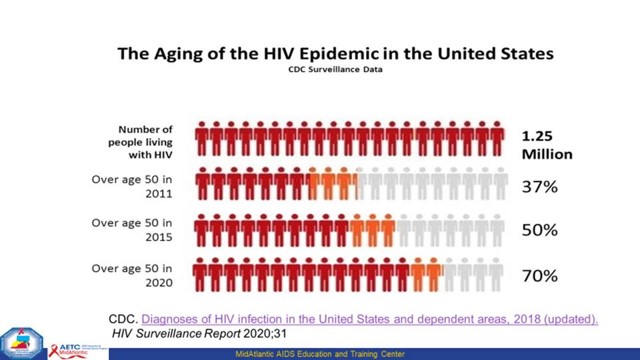
As PLWH age, they experience an array of new difficulties, including higher rates and earlier onset of comorbidities, mental health issues, geriatric syndromes, ageism, and stigma. Older adults may be less aware of their HIV risk and receive a late diagnosis. Among older PLWH in 2015, 95% were aware of their infection, 69% received care, 56% were received ongoing medical care, and 60% were virally suppressed.
Social determinants of health (SDOH) are defined as “the circumstances in which people are born, grow up, live, work and age, and the systems put in place to deal with illness.” SDOH can include housing, access to insurance, access to competent medical care, and financial stability for PLWH. The importance of these social determinants is amplified among those aging with HIV. For example, stigma may create barriers to quality care. According to one global survey in 2016, 82% of 1111 PLWH had experienced stigma related to their HIV status in the previous 12 months. In healthcare settings, stigma and discrimination associated with HIV may discourage people from getting tested and knowing their status, sharing their HIV status with others, initiating HIV care and treatment early, and adhering to treatment, necessary to protect the individual and public health.
The health care and social needs of this growing population are complex and change as individuals are living longer with HIV. Federal programs that serve older adults must consider older adults living with HIV as a chronic disease. There must be a stronger focus on quality of life and integrating a framework that will promote and sustain the needs of this overlooked population, including empower people to address HIV discrimination; enacting protective laws; and training the healthcare workforce to deliver standardized, nondiscriminatory, confidential, patient-centric care.
Tune in to TFAH’s April AFPHS Training for more information on:
- Describing the epidemiology of HIV in older adults
- Describing the evolving landscape of HIV and aging
- Reviewing the impact of the SDOH on a growing population of older adults with HIV, and
- Discussing what can be done to improve overall health outcomes of PLWH