Elder Mistreatment Prevention Toolkit for Public Health

Introduction
Elder mistreatment (EM) prevention is fundamentally an issue of the public’s health and, as such, the public health sector is taking action to prevent mistreatment and coordinate support for victims. Elder mistreatment affects the health, safety, and well-being of older adults, their families, and the communities in which they live. It can have profound and long-term impacts on the emotional, mental, physical, and financial health of victims.
Public health practitioners often have key roles in the prevention of elder mistreatment, including community leaders, conveners, and trusted sources of information. However, many lack extensive knowledge of the resources that may be available to them to both prevent elder mistreatment and support victims and their families.
Trust for America’s Health partnered with the Education Development Center and the National Alliance for Caregiving to build this toolkit to support the public health sector in preventing EM and working with community partners to help victims, families, and perpetrators.
Using The Toolkit
Who Should Use the Toolkit?
Public health leaders, staff, and practitioners; public health partners such as aging services personnel and community health workers; multidisciplinary teams (community-based teams that may include public health, emergency services, police, adult protective services, mental health providers, and others); other state or local agency staff who are part of your internal team.
Why Should We Use the Toolkit?
The Elder Mistreatment Prevention Toolkit is designed to build awareness and understanding of the public health roles in improving understanding and awareness of elder mistreatment, and to build strategies to prevent mistreatment and mitigate its effects when it does occur. Each section includes a list of strategies, tools, and programs, along with resources for building awareness.
How Should We Use the Toolkit?
Public health practitioners and partners are encouraged to access and review the six components that align with the Age-Friendly Public Health Systems 6Cs Framework, either sequentially or in whatever order is most expeditious for your learning experience. From there, teams and partners can build a strategy or plan, including a timeline for implementation. Teams could focus on one of the 6Cs, or select strategies across each of the 6Cs, depending on the community’s needs, assets, and readiness for implementation.
Facts on Elder Mistreatment


Making the Case: Elder Mistreatment is a Preventable Public Health Concern
What makes prevention of elder mistreatment an important societal issue?
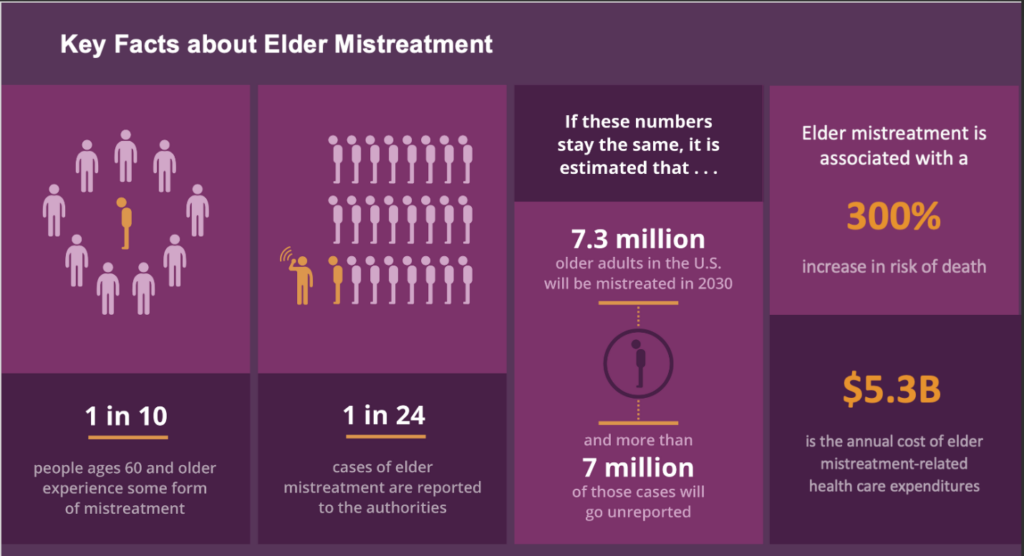
Elder mistreatment is not an inevitable consequence of aging—it is a preventable issue that can be addressed through education, coordinated services, and person-centered programs. Unfortunately, it is an issue that the public perceives as isolated, or that may be associated with dementia or other aging issues. In reality, one in every 10 people is likely to experience elder mistreatment in their lifetime, making it a real threat and one that impacts the health and well-being of millions of Americans. By addressing elder mistreatment through targeted public health strategies, we can reduce the emotional, mental, physical, and financial burdens that victims and their support networks endure over time.
Why should public health practitioners address elder mistreatment?
Example Quote from a Public Health Department Worker:
“[The public health department has] the ability and opportunities to come in contact with vulnerable populations through our work, our direct work with the older adults through some of the education that we do in the community. Somebody could self-disclose to us that they’re in a . . . bad situation through our housing department . . . and [the department workers] may identify people who, you know, are also being neglected or not cared for. So I think that we have many touch points as a public health entity in which we come in contact with vulnerable people, including older adults.”
Public health professionals bring a unique blend of expertise and community insight that is critical in addressing elder mistreatment. Their training in epidemiology, community assessment, and health promotion positions them to:
- Identify risk factors and trends: Leveraging data and research, practitioners can pinpoint communities at higher risk and implement preventive strategies before mistreatment occurs.
- Serve as community conveners: Public health departments can mobilize a wide range of partners and collaborators—like local community organizations, county departments, and healthcare providers—to collaborate on comprehensive prevention and intervention initiatives.
- Disseminate accurate information: Public health professionals are uniquely qualified to provide evidence-based guidance and resources that inform both prevention efforts and victim support.
- Develop and implement programs: Drawing on their public health skill set, public health professionals can design, test, and refine programs that effectively address elder mistreatment while also integrating with existing public health services.
Despite these crucial roles, many public health practitioners may not yet be fully aware of the scope of their potential impact on elder mistreatment prevention. They might also lack access to the specific resources, tools, and training needed to translate their skills into effective action. This toolkit aims to bridge that gap—empowering practitioners with the necessary knowledge, strategies, and best practices to champion elder mistreatment prevention in their communities.
Elder Mistreatment Risk Factors
Conversations with key informants from public health validated research data on several key factors that increase the risk of elder mistreatment:
- Cognitive and Physical Decline: Older adults experiencing cognitive impairment (e.g., dementia or Alzheimer’s disease) or physical limitations face higher risks of mistreatment. Cognitive and physical decline can impact older adults’ ability to recognize, prevent, or report harm. It can also reduce the likelihood that their reports are taken seriously.
- Financial Strain: Financial strain within families or experienced by caregivers significantly increases the risk of elder mistreatment. Limited financial resources, coupled with stress over financial responsibilities, may heighten the likelihood of neglect, financial exploitation, or emotional and physical abuse.
- Caregiver Strain: Caregiver strain, often resulting from stress, burnout, or insufficient resources, can increase the risk that a caregiver may perpetrate mistreatment. Additional factors may include family dysfunction and complex medical conditions. Support and resources for caregivers are essential protective factors.
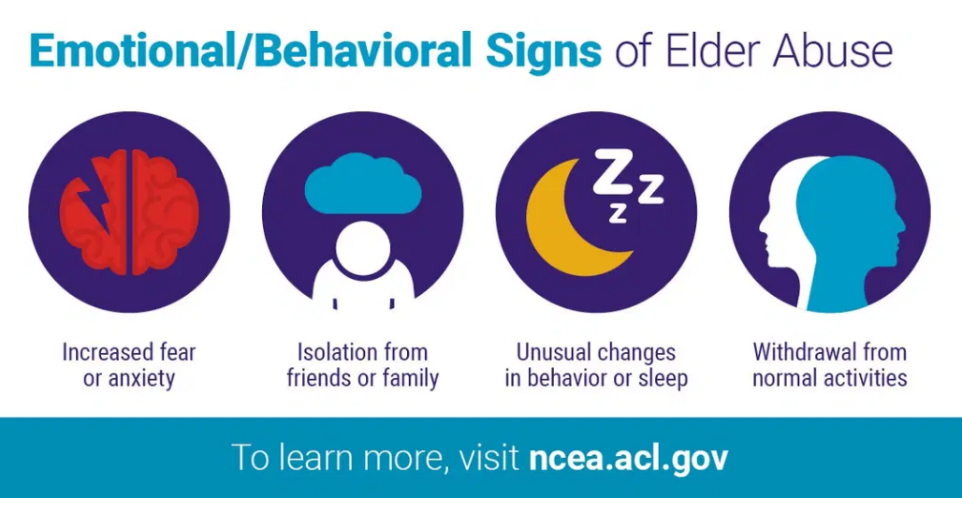
- Social Isolation: Social isolation substantially elevates the risk of elder mistreatment by reducing elders’ access to supportive networks, advocacy, and oversight. Isolation makes detecting and reporting mistreatment challenging, allowing abuse and exploitation to persist unnoticed.
- Financial Gain: The potential for financial gain can function as a motive to exploit older adults. Financial abuse may range from theft and fraud to coerced property transfers or undue influence. The person exploiting the older adult may be a trusted person in their life or a stranger, creating additional challenges in addressing financial exploitation.
- Evolving Scams: Scams targeting older adults continually evolve, exploiting technological advances such as AI, as well as social dynamics. Elderly individuals, especially those isolated or unfamiliar with modern technology, may be particularly vulnerable. Awareness-raising and education serve as protective strategies against such exploitation.
- Ageism: Ageism—discrimination or prejudice against individuals due to their age—underpins many forms of elder mistreatment. Societal attitudes that devalue older adults or dismiss their needs contribute to environments in which mistreatment may occur more frequently or go unnoticed. Combating ageism through education and advocacy serves as a protective measure.
Public health professionals can work to mitigate these risk factors and build supportive systems in partnership with community or state level agencies. Strategies to do so can be found in the 6Cs guidance documents included in this toolkit.
Importance of Supporting Caregivers as a Prevention Strategy
Supporting Caregivers: A Prevention Strategy for Elder Mistreatment
The mental health and financial burdens on caregivers significantly impact the quality of care they can provide. According to Caregiving in the U.S. 2025, in 2025, 63 million American adults provided ongoing care to adults or children with a medical condition or disability, representing almost one-quarter of all adults in the United States—a 45 percent increase since 2015. Women account for 61% of family caregivers. 61% of family caregivers identify as white (non-Latino), 16% as Hispanic or Latino, 13% as African American or Black (non-Latino), and 6% as Asian American or Pacific Islander. 59 million family caregivers provide care to an adult with a complex medical condition or disability. Caregivers are increasingly responsible for adults with multiple chronic health conditions, including long-term physical conditions (63%), emotional or mental health issues (27%), and memory problems such as dementia (26%). These rising demands place immense strain on caregivers, with 45% experience physical strain and 64% reporting their caregiving situation as highly stressful.
These stressors make it difficult for caregivers to maintain their own physical and emotional health, which in turn can compromise their ability to provide optimal care. 45% of caregivers are in high-intensity caregiving situations, providing more than 24 hours of care each week, while 61% work outside the home while caregiving. Financial challenges further compound the burden, with 47% of caregivers facing significant financial impacts, such as going into debt or struggling to pay bills. Despite these challenges, many caregivers take on this role without access to adequate and affordable services or supports. More than half (55%) perform medical and nursing tasks, yet only 22% receive training for these complex tasks.
The growing complexity of care recipients’ needs underscores the importance of equipping caregivers with the resources necessary to manage their responsibilities effectively while maintaining their own well-being. Reducing a caregiver’s strain can lower the risk that the caregiver perpetrates abuse. Also, if the caregiver is an older adult, reducing the caregiver’s strain can reduce the risk of the caregiver becoming a victim of abuse.
For more information about how the public health sector can support caregivers, please see Trust for America’s Health’s brief, Public Health Roles in Supporting Family Caregivers.
Methodology
An environmental scan was conducted that included a review of published literature and other resources to identify definitions of elder mistreatment, risk factors, screening tools, prevention strategies, and intervention programs and tools.
Individual interviews were conducted with 17 professionals who have worked in elder mistreatment or public health research, advocacy, and direct services. Nine interviewees had expertise in policy and advocacy, three were researchers, four were public health workers, and one was a medical practitioner. Participants were asked to share their perspectives on elder mistreatment as a public health issue, factors affecting risk of elder mistreatment, and aspects of public health’s role in addressing and preventing elder mistreatment. Participants were also asked about innovative approaches and solutions they were aware of in public health practice. Additionally, participants were asked to describe factors that prohibited or supported public health’s involvement in addressing and preventing elder mistreatment. Interviews were conducted virtually between June and August 2024 by five project staff. Interviews lasted for about an hour each. Each interview was video recorded, transcribed, and analyzed. Coding was completed in Dedoose Qualitative Analysis Software. An initial coding scheme was developed based on the interview guide. A project staff member applied the coding scheme to the transcripts and presented the results to the rest of the team to assess If any themes were missing. Using Braun and Clark’s approach to thematic analysis, codes were analyzed and grouped into themes (Braun & Clarke, 2006). Project staff used the themes and key informant recommendations to identify strategies and resources aligned with each of the 6Cs.

The AFPHS 6Cs Training and Implementation Guide was developed by Trust for America’s Health with funding from The John A. Hartford Foundation and in partnership with the Education Development Center and the National Alliance for Caregiving.